Classification of Spaces in Healthcare Facilities ?
Healthcare facilities can be broadly classified based on the types of services they offer:
- Hospitals: These are large facilities that offer a wide range of services, including emergency care, surgery, inpatient care, diagnostic testing, and therapy. Hospitals can be further classified based on their size, ownership (e.g., public, private, non-profit), and teaching status.
- Clinics: Clinics are typically smaller than hospitals and focus on providing outpatient care. They may be specialized in a particular area of medicine, such as primary care, cardiology, or dermatology.
- Ambulatory Surgical Centers (ASCs): ASCs provide surgical procedures on an outpatient basis, meaning patients do not stay overnight. They are often more cost-effective than hospitals for certain procedures.
- Long-Term Care Facilities: These facilities provide care for individuals who need assistance with daily living activities over an extended period. They include nursing homes, assisted living facilities, and rehabilitation centers.
- Specialty Care Facilities: These facilities focus on providing care for specific conditions or populations, such as cancer centers, psychiatric hospitals, and children’s hospitals.
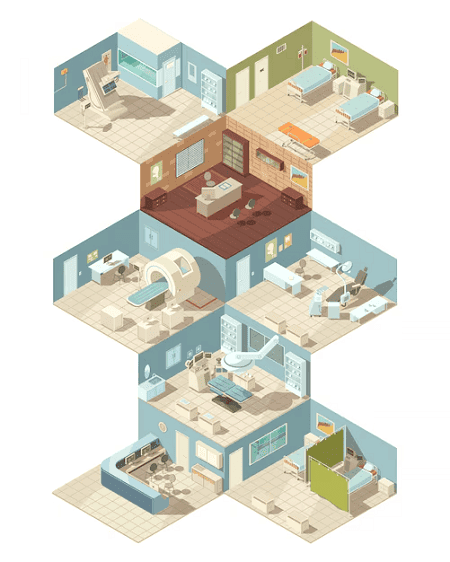
Within each of these facility types, spaces can be further classified based on their function:
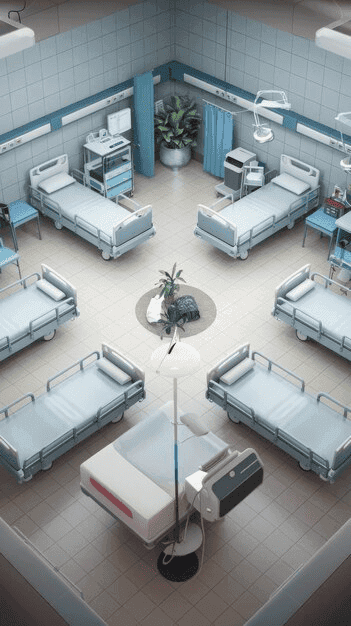
- Patient care areas: These include exam rooms, treatment rooms, operating rooms, patient rooms, and waiting areas.
- Diagnostic and treatment areas: These include radiology departments, laboratories, pharmacies, and therapy areas.
- Support areas: These include administrative offices, staff lounges, storage areas, and building services.
The classification of spaces in healthcare facilities is important for several reasons:
- It helps to ensure that facilities are designed and operated efficiently. By understanding the different types of spaces needed, healthcare providers can optimize the use of their resources.
- It helps to ensure patient safety. Proper classification of spaces can help to prevent the spread of infection and other hazards.
- It helps to ensure compliance with regulations. There are many regulations that govern the design and operation of healthcare facilities, and these regulations often vary depending on the type of space.
In addition to the classifications mentioned above, healthcare facilities can also be classified based on their level of care. For example, a primary care clinic provides a different level of care than a tertiary care hospital. The level of care provided by a facility will affect the types of spaces that are needed.
Overall, the classification of spaces in healthcare facilities is a complex topic. There are many different ways to classify spaces, and the best approach will vary depending on the specific facility.
What is Classification of Spaces in Healthcare Facilities ?
Healthcare facilities are complex environments with a variety of spaces designed to support different functions and activities. Classifying these spaces is essential for efficient design, operation, and regulatory compliance. Here’s a breakdown of how spaces in healthcare facilities are classified:
1. Based on Service Type:
- Hospitals: Offer a wide range of services, including emergency care, surgery, inpatient care, diagnostics, and therapy.
- Clinics: Focus on outpatient care, often specializing in a particular area of medicine.
- Ambulatory Surgical Centers (ASCs): Provide outpatient surgical procedures.
- Long-Term Care Facilities: Offer extended care for individuals needing assistance with daily living.
- Specialty Care Facilities: Focus on specific conditions or populations (e.g., cancer centers, psychiatric hospitals).
2. Based on Function:
- Patient Care Areas: Exam rooms, treatment rooms, operating rooms, patient rooms, waiting areas.
- Diagnostic and Treatment Areas: Radiology departments, laboratories, pharmacies, therapy areas.
- Support Areas: Administrative offices, staff lounges, storage areas, building services.
3. Based on Level of Care:
- Primary Care: Focuses on prevention and basic medical needs.
- Secondary Care: Involves specialists and hospitals for more complex conditions.
- Tertiary Care: Highly specialized care provided in major medical centers.
Importance of Classification:
- Efficient Design and Operation: Optimizes resource use.
- Patient Safety: Helps prevent infection and other hazards.
- Regulatory Compliance: Ensures adherence to relevant standards.
Additional Considerations:
- Flexibility: Spaces should be adaptable to changing needs.
- Technology Integration: Spaces need to accommodate evolving technology.
- Patient Experience: Design should promote comfort and well-being.
Key Standards and Guidelines:
- Facility Guidelines Institute (FGI): Provides guidelines for healthcare facility design and construction.
- ASHRAE Standard 170: Sets ventilation standards for healthcare facilities.
- NFPA 99: Addresses healthcare facilities’ fire safety and electrical safety.
In Conclusion:
Classifying spaces in healthcare facilities is a multifaceted process that considers various factors, including service type, function, level of care, and specific needs. Effective classification is crucial for creating safe, efficient, and patient-centered healthcare environments.
Who is required Classification of Spaces in Healthcare Facilities ?
The classification of spaces in healthcare facilities is important for a variety of stakeholders, including:
- Healthcare providers: Proper classification of spaces can help healthcare providers to optimize the use of their resources, ensure patient safety, and comply with regulations.
- Architects and designers: Architects and designers need to understand the different types of spaces needed in a healthcare facility in order to design efficient and functional facilities.
- Construction companies: Construction companies need to understand the different types of spaces in order to build facilities that meet the needs of healthcare providers and patients.
- Regulatory agencies: Regulatory agencies need to classify spaces in order to ensure that healthcare facilities are designed and operated safely and efficiently.
- Patients: Patients benefit from proper classification of spaces because it helps to ensure that they receive care in a safe and comfortable environment.
Here are some specific examples of how different stakeholders use the classification of spaces in healthcare facilities:
- Healthcare providers use the classification of spaces to determine staffing needs, allocate resources, and develop emergency plans.
- Architects and designers use the classification of spaces to design facilities that meet the needs of healthcare providers and patients. For example, they need to know the different types of patient care areas in order to design efficient and functional spaces.
- Construction companies use the classification of spaces to build facilities that meet the needs of healthcare providers and patients. For example, they need to know the different types of diagnostic and treatment areas in order to install the necessary equipment.
- Regulatory agencies use the classification of spaces to ensure that healthcare facilities are designed and operated safely and efficiently. For example, they may require that certain types of spaces meet specific ventilation or fire safety requirements.
- Patients benefit from proper classification of spaces because it helps to ensure that they receive care in a safe and comfortable environment. For example, patients are more likely to feel comfortable in a waiting area that is designed to be welcoming and relaxing.
Overall, the classification of spaces in healthcare facilities is important for a variety of stakeholders. By understanding the different types of spaces needed, healthcare providers, architects, designers, construction companies, regulatory agencies, and patients can work together to create safe, efficient, and comfortable healthcare environments.
When is required Classification of Spaces in Healthcare Facilities ?
The classification of spaces in healthcare facilities is required at several key stages:
1. Planning and Design:
- New Construction: When building a new healthcare facility, classifying spaces is crucial from the initial planning stages. It informs the architectural design, ensuring that the facility meets the functional needs of its intended services and complies with regulations.
- Renovation or Expansion: When renovating or expanding an existing facility, space classification helps determine how the new or modified spaces will integrate with the existing layout and functionality. It ensures that the changes meet current standards and regulations.
2. Regulatory Compliance:
- Licensing and Accreditation: Healthcare facilities must comply with various regulations and standards to obtain licenses and accreditation. Space classification is essential for demonstrating compliance with these requirements, which often specify design and operational criteria for different types of spaces.
- Building Codes: Building codes, such as the International Building Code (IBC) and NFPA 101 Life Safety Code, classify spaces based on occupancy and use. This classification determines the applicable fire safety, accessibility, and other building requirements.
3. Operational Efficiency:
- Space Allocation: Proper classification helps optimize space utilization, ensuring that each area is used effectively for its intended purpose. This is crucial for efficient workflow, resource allocation, and cost management.
- Staffing and Equipment: Space classification informs staffing needs and equipment requirements for different areas. For example, operating rooms require specialized equipment and staff compared to waiting areas.
4. Patient Safety:
- Infection Control: Classifying spaces based on their function and risk level is crucial for infection control. It helps determine appropriate ventilation, cleaning protocols, and other measures to minimize the spread of infections.
- Emergency Preparedness: Space classification plays a role in emergency planning, such as evacuation routes, fire suppression systems, and disaster preparedness strategies.
5. Continuous Improvement:
- Performance Evaluation: Classifying spaces allows healthcare facilities to track and evaluate the performance of different areas. This data can be used to identify areas for improvement in design, operations, and patient care.
- Adaptability: Healthcare needs and technologies evolve. Space classification helps ensure that facilities can adapt to these changes by understanding the function and requirements of different spaces.
In summary, the classification of spaces in healthcare facilities is an ongoing process that starts with planning and design and continues throughout the facility’s lifecycle. It is essential for regulatory compliance, operational efficiency, patient safety, and continuous improvement.
COURTESY : Kelli Belanger
Where is required Classification of Spaces in Healthcare Facilities ?
The classification of spaces in healthcare facilities is required in a variety of settings and contexts, including:
1. Healthcare Facilities Themselves:
- Hospitals: Classification is crucial for all departments, from emergency rooms and operating theaters to patient wards and diagnostic imaging.
- Clinics: Whether primary care or specialized, clinics need to classify spaces for efficient patient flow, infection control, and regulatory compliance.
- Ambulatory Surgical Centers (ASCs): ASCs require careful classification of procedure rooms, recovery areas, and support spaces to ensure patient safety and operational efficiency.
- Long-Term Care Facilities: Nursing homes and assisted living facilities need to classify spaces for resident care, dining, recreation, and staff support.
- Specialty Care Facilities: Cancer centers, psychiatric hospitals, and other specialized facilities require classification tailored to their unique needs.
2. Design and Construction:
- Architectural Firms: Architects use space classification to design functional and compliant healthcare facilities.
- Engineering Firms: Engineers rely on space classification to design appropriate HVAC, electrical, and plumbing systems.
- Construction Companies: Builders use space classification to understand the requirements for each area and ensure proper construction.
3. Regulatory and Accreditation Bodies:
- Government Agencies: Health departments and building code officials use space classification to enforce regulations and ensure safety.
- Accreditation Organizations: Organizations like The Joint Commission use space classification as part of their accreditation process.
4. Other Stakeholders:
- Healthcare Consultants: Consultants use space classification to advise healthcare providers on facility planning and operations.
- Researchers: Researchers may use space classification to study healthcare facility design and its impact on patient outcomes.
- Insurance Companies: Insurers may use space classification to assess risk and determine coverage for healthcare facilities.
In essence, the classification of spaces in healthcare facilities is relevant wherever healthcare services are provided, designed, regulated, or studied. It is a fundamental tool for ensuring the safety, efficiency, and effectiveness of healthcare environments.
How is required Classification of Spaces in Healthcare Facilities ?
The classification of spaces in healthcare facilities is a structured process that involves several key steps:
1. Identifying the Purpose and Function of Each Space:
- Detailed Inventory: Begin by creating a comprehensive list of all spaces within the facility, from patient rooms and operating theaters to waiting areas and administrative offices.
- Functional Analysis: For each space, determine its primary purpose and the activities that will take place there. Consider factors like patient care, diagnostics, treatment, support services, and administrative functions.
2. Applying Relevant Classification Systems:
- Service Type: Classify spaces based on the type of healthcare service they support (e.g., hospital, clinic, long-term care).
- Function: Categorize spaces based on their specific function (e.g., patient care, diagnostic/treatment, support).
- Level of Care: Consider the level of care provided in each space (e.g., primary, secondary, tertiary).
- Occupancy Classification: Refer to building codes (e.g., IBC) to classify spaces based on occupancy and use (e.g., patient care, ambulatory care, business).
3. Considering Specific Requirements and Standards:
- Regulatory Compliance: Ensure that the classification aligns with relevant regulations and standards (e.g., licensing requirements, building codes, fire safety codes).
- Healthcare Guidelines: Consult industry guidelines and best practices, such as those provided by the Facility Guidelines Institute (FGI) and ASHRAE.
- Infection Control: Classify spaces based on infection risk and determine appropriate ventilation, cleaning, and other control measures.
- Accessibility: Ensure that the classification considers accessibility requirements for patients, staff, and visitors with disabilities.
4. Documenting and Communicating the Classification:
- Detailed Records: Maintain accurate records of the classification for each space, including its purpose, function, and any specific requirements.
- Clear Communication: Communicate the classification to all relevant stakeholders, including healthcare providers, architects, engineers, and construction teams.
- Signage and Labeling: Use clear signage and labeling within the facility to identify the classification of different spaces.
5. Reviewing and Updating the Classification:
- Ongoing Process: Space classification should be an ongoing process, with regular reviews and updates as needed.
- Changes in Needs: Re-evaluate the classification when there are changes in healthcare services, technology, or patient needs.
- Feedback and Input: Seek feedback from healthcare providers and other stakeholders to ensure that the classification remains accurate and relevant.
By following these steps, healthcare facilities can effectively classify their spaces to support efficient operations, patient safety, regulatory compliance, and continuous improvement.
Case study is Classification of Spaces in Healthcare Facilities ?
Case Study: Classification of Spaces in a New Outpatient Clinic
Scenario: A healthcare provider is building a new outpatient clinic specializing in cardiology. They need to classify the spaces within the clinic to ensure efficient design, regulatory compliance, and patient safety.
1. Identifying Spaces and Functions:
The clinic will include:
- Waiting area: For patients awaiting appointments.
- Reception area: For patient check-in and check-out.
- Exam rooms (3): For patient consultations and examinations.
- Treatment room: For minor procedures and tests.
- Diagnostic area: For echocardiograms and other tests.
- Staff area: Including a break room and workstations.
- Administrative offices: For clinic management.
- Restrooms: For patients and staff.
2. Applying Classification Systems:
- Service Type: Clinic
- Function:
- Patient care: Exam rooms, treatment room, diagnostic area.
- Support: Waiting area, reception, restrooms.
- Administrative: Staff area, administrative offices.
- Level of Care: Primary/Secondary (depending on the scope of services).
- Occupancy Classification (IBC):
- Exam/treatment rooms: Business (B) or Ambulatory Care (I-2) depending on local code interpretation.
- Waiting area: Assembly (A)
- Offices: Business (B)
3. Considering Requirements and Standards:
- Regulatory Compliance:
- Ensure compliance with ADA for accessibility in all areas.
- Meet local building codes for fire safety and occupancy.
- Adhere to HIPAA for patient privacy in exam rooms and reception.
- Healthcare Guidelines:
- Consult FGI guidelines for space sizes and design recommendations.
- Refer to ASHRAE 170 for ventilation requirements in exam and treatment rooms.
- Infection Control:
- Classify exam and treatment rooms as higher risk for infection control.
- Ensure proper handwashing facilities and waste disposal in these areas.
- Patient Experience:
- Design the waiting area to be comfortable and welcoming.
- Ensure clear wayfinding and signage throughout the clinic.
4. Documentation and Communication:
- Space Classification Schedule: Create a document listing each space, its classification, and relevant requirements.
- Floor Plans: Clearly label each space on the floor plans with its classification.
- Construction Documents: Incorporate the classification into the construction documents for bidding and building.
5. Review and Updates:
- Regular Review: Review the space classification periodically to ensure it still meets the clinic’s needs.
- Flexibility: Design spaces to be adaptable to future changes in technology or service offerings.
Outcome:
By classifying spaces effectively, the clinic can:
- Optimize workflow: Ensure efficient movement of patients and staff.
- Enhance patient safety: Implement appropriate infection control and safety measures.
- Comply with regulations: Meet all necessary building codes and healthcare standards.
- Create a positive environment: Design a comfortable and welcoming space for patients and staff.
This case study demonstrates the importance and process of classifying spaces in a healthcare facility. It highlights how this process contributes to creating a safe, efficient, and patient-centered environment.
COURTESY : Anixter
White paper on Classification of Spaces in Healthcare Facilities ?
White Paper: Classification of Spaces in Healthcare Facilities: A Foundation for Design, Operation, and Patient Care
Abstract:
Healthcare facilities are complex environments designed to deliver a wide range of services. Effective classification of spaces within these facilities is crucial for optimizing design, ensuring regulatory compliance, promoting patient safety, and streamlining operations. This white paper explores the rationale, methodologies, and benefits of space classification in healthcare, highlighting best practices and emerging trends.
1. Introduction:
Healthcare facilities, encompassing hospitals, clinics, ambulatory surgical centers, and long-term care facilities, are intricate ecosystems. Each space within these facilities serves a specific purpose, contributing to the overall patient care experience. A well-defined system for classifying these spaces is essential for various stakeholders, including architects, designers, healthcare providers, regulatory bodies, and, ultimately, patients.
2. Rationale for Space Classification:
The classification of spaces in healthcare facilities serves several critical functions:
- Optimized Design: Architects and designers utilize space classifications to create functional and efficient layouts. Understanding the intended use and required adjacencies of different spaces enables them to optimize workflows and resource allocation.
- Regulatory Compliance: Healthcare facilities must adhere to various building codes, fire safety regulations, and accreditation standards. Space classification is fundamental for demonstrating compliance with these requirements, which often stipulate specific design criteria for different types of spaces.
- Enhanced Patient Safety: Proper classification facilitates the implementation of appropriate safety measures. For example, spaces designated for surgical procedures have stringent infection control and ventilation requirements compared to waiting areas.
- Streamlined Operations: Clear space classifications enable efficient resource allocation, staffing decisions, and maintenance protocols. Knowing the function and occupancy of each space allows for targeted resource deployment.
- Improved Patient Experience: Thoughtful space classification contributes to a positive patient experience. Well-designed waiting areas, comfortable examination rooms, and easy wayfinding enhance patient satisfaction and reduce anxiety.
3. Methodologies for Space Classification:
Several classification systems are employed in healthcare, often used in conjunction:
- Service Type: Categorizing facilities by the type of care provided (e.g., hospital, clinic, long-term care).
- Function: Classifying spaces based on their primary activity (e.g., patient care, diagnostics, administration).
- Level of Care: Differentiating spaces based on the intensity of care provided (e.g., primary, secondary, tertiary).
- Occupancy Classification (IBC): Utilizing the International Building Code’s occupancy classifications (e.g., Business, Ambulatory Care, Assembly) for regulatory compliance.
- Infection Control Risk Assessment: Classifying spaces based on the potential for infection transmission to guide cleaning, ventilation, and other infection control measures.
4. Best Practices in Space Classification:
- Comprehensive Inventory: Begin with a detailed inventory of all spaces within the facility, documenting their dimensions, intended use, and equipment requirements.
- Collaboration: Engage all stakeholders, including healthcare providers, architects, engineers, and facility managers, in the classification process.
- Compliance with Standards: Adhere to relevant building codes, healthcare guidelines (e.g., FGI), and accreditation standards.
- Flexibility and Adaptability: Design spaces to accommodate future changes in technology, healthcare practices, and patient needs.
- Documentation and Communication: Maintain clear and accessible documentation of space classifications and communicate this information effectively to all stakeholders.
5. Emerging Trends:
- Evidence-Based Design: Integrating research and data on the impact of design on patient outcomes to inform space classification and design decisions.
- Technology Integration: Designing spaces to seamlessly accommodate evolving medical technologies and data management systems.
- Patient-Centered Design: Prioritizing patient comfort, privacy, and accessibility in the classification and design of spaces.
- Sustainability: Incorporating sustainable design principles in the construction and operation of healthcare spaces.
6. Conclusion:
The classification of spaces in healthcare facilities is a fundamental process that underpins effective design, regulatory compliance, patient safety, and operational efficiency. By adhering to best practices and embracing emerging trends, healthcare providers can create environments that support the delivery of high-quality, patient-centered care. Continuous review and adaptation of space classifications are essential to ensure that healthcare facilities remain functional, safe, and responsive to the evolving needs of patients and the healthcare industry.
Industrial application of Classification of Spaces in Healthcare Facilities ?
While the classification of spaces in healthcare facilities might seem like an abstract concept, it has significant industrial applications that impact various sectors:
1. Construction and Design:
- Standardized Design Templates: Classification systems enable the development of standardized design templates for different healthcare spaces. This streamlines the architectural and engineering process, reducing design time and costs.
- Modular Construction: Classified spaces can be designed and constructed modularly, allowing for faster and more efficient construction. This is particularly useful for expanding existing facilities or building temporary healthcare structures.
- Cost Estimation: Accurate space classification facilitates precise cost estimation for construction projects. By understanding the specific requirements of each space, contractors can provide more accurate bids and manage budgets effectively.
2. Manufacturing and Supply Chain:
- Specialized Equipment: Manufacturers of medical equipment can tailor their products to the specific needs of different space classifications. For example, they can develop specialized ventilation systems for operating rooms or patient lifts for long-term care facilities.
- Supply Chain Optimization: Classifying spaces helps optimize the supply chain for medical supplies and equipment. Distributors can anticipate demand for specific products based on the types of spaces being built or renovated.
- Inventory Management: Healthcare facilities can use space classification to improve inventory management. By knowing the specific supplies and equipment required for each space, they can optimize stock levels and reduce waste.
3. Technology and Software:
- Building Management Systems (BMS): Space classification is integrated into BMS to monitor and control environmental conditions, such as temperature, humidity, and ventilation, in different areas. This ensures optimal conditions for patient care and staff comfort.
- Space Planning Software: Software tools utilize space classification to help healthcare providers optimize space utilization, plan renovations, and manage facility resources effectively.
- Healthcare IT Systems: Electronic health records (EHR) and other healthcare IT systems can be linked to space classifications to track patient flow, allocate resources, and improve operational efficiency.
4. Consulting and Services:
- Healthcare Facility Planning: Consultants use space classification to advise healthcare providers on facility planning, design, and operations. They help optimize space utilization, improve workflow, and ensure regulatory compliance.
- Facility Management Services: Companies providing facility management services can leverage space classification to tailor their services to the specific needs of different areas, such as cleaning, maintenance, and security.
- Training and Education: Space classification is incorporated into training programs for healthcare professionals, architects, engineers, and facility managers to ensure a common understanding of healthcare facility design and operations.
5. Real Estate and Investment:
- Valuation of Healthcare Properties: Space classification is a key factor in the valuation of healthcare properties. Investors and developers use this information to assess the potential of a property and make informed decisions.
- Market Analysis: Understanding the distribution of different space classifications in a region helps analyze the healthcare market and identify opportunities for new facilities or specialized services.
In conclusion, the classification of spaces in healthcare facilities has far-reaching industrial applications that extend beyond the healthcare sector itself. It impacts construction, manufacturing, technology, consulting, and real estate, contributing to the development of efficient, safe, and patient-centered healthcare environments.
Research and development of Classification of Spaces in Healthcare Facilities ?
Research and development in the classification of spaces in healthcare facilities is an ongoing process, driven by the need to create more efficient, safe, and patient-centered environments. Here are some key areas of focus:
1. Developing More Granular and Dynamic Classification Systems:
- Beyond Basic Categories: Current classification systems often rely on broad categories. Research is exploring more granular classifications that consider specific activities, patient populations, and technology integration within spaces.
- Dynamic Classification: Healthcare needs and technologies evolve rapidly. Research is focused on developing dynamic classification systems that can adapt to these changes and allow for flexible space utilization.
- Data-Driven Classification: Utilizing data analytics and machine learning to analyze space usage patterns and inform classification decisions. This can lead to more evidence-based and optimized space allocation.
2. Integrating Technology into Space Classification:
- Smart Building Technologies: Integrating sensors, IoT devices, and building management systems to collect data on space usage, environmental conditions, and equipment performance. This data can be used to refine space classifications and optimize building operations.
- Digital Twins: Creating digital models of healthcare facilities that incorporate space classifications and allow for virtual simulations and analysis. This can help evaluate design options, optimize workflows, and improve space utilization.
- AI-Powered Classification: Exploring the use of artificial intelligence and machine learning to automate space classification based on data analysis and predictive modeling.
3. Focusing on Patient-Centered Design:
- Impact of Space on Patient Outcomes: Research is investigating the relationship between space classification and patient outcomes, such as healing rates, infection rates, and patient satisfaction. This can inform the design of spaces that promote well-being and recovery.
- Personalized Spaces: Exploring the concept of personalized spaces that can be adapted to individual patient needs and preferences. This may involve using technology to adjust lighting, temperature, and other environmental factors.
- Inclusive Design: Research is focused on developing classification systems that consider the needs of diverse patient populations, including those with disabilities, cultural differences, and specific health conditions.
4. Addressing Emerging Challenges:
- Infection Control: Research is crucial in classifying spaces based on infection risk and developing effective strategies to minimize the spread of infections. This includes studying ventilation systems, cleaning protocols, and the use of antimicrobial materials.
- Mental Health: The design of mental health facilities requires specialized space classifications that promote safety, privacy, and therapeutic environments. Research is exploring how space can impact patient well-being and recovery in these settings.
- Telehealth Integration: As telehealth becomes more prevalent, research is needed to understand how to integrate telehealth spaces into healthcare facilities and how to classify these spaces effectively.
5. Collaborative Research and Knowledge Sharing:
- Interdisciplinary Collaboration: Research in space classification requires collaboration between architects, engineers, healthcare professionals, researchers, and technology experts.
- Open Data and Knowledge Sharing: Sharing research findings and best practices through publications, conferences, and online platforms is essential to advance the field and improve healthcare facility design.
By focusing on these areas of research and development, the field of space classification in healthcare facilities can continue to evolve and contribute to the creation of innovative, efficient, and patient-centered healthcare environments.
COURTESY : Principles of Health Science
References
- ^ “Hospitals”. World Health Organization. Retrieved 24 January 2018.
- ^ Jump up to:a b c “India’s ‘production line’ heart hospital”. bbcnews.com. 1 August 2010. Archived from the original on 18 April 2017. Retrieved 13 October 2013.
- ^ Hall, Daniel (December 2008). “Altar and Table: A phenomenology of the surgeon-priest”. Yale Journal of Biology and Medicine. 81 (4): 193–98. PMC 2605310. PMID 19099050.
Although physicians were available in varying capacities in ancient Rome and Athens, the institution of a hospital dedicated to the care of the sick was a distinctly Christian innovation rooted in the monastic virtue and practise of hospitality. Arranged around the monastery were concentric rings of buildings in which the life and work of the monastic community was ordered. The outer ring of buildings served as a hostel in which travellers were received and boarded. The inner ring served as a place where the monastic community could care for the sick, the poor and the infirm. Monks were frequently familiar with the medicine available at that time, growing medicinal plants on the monastery grounds and applying remedies as indicated. As such, many of the practicing physicians of the Middle Ages were also clergy.
- ^ Lovoll, Odd (1998). A Portrait of Norwegian Americans Today. U of Minnesota Press. p. 192. ISBN 978-0-8166-2832-2.
- ^ Cassell’s Latin Dictionary, revised by J. Marchant & J. Charles, 260th. thousand.
- ^ Jump up to:a b c d e “Our Background”. District Hospital Leadership Forum. Archived from the original on 14 July 2014. Retrieved 10 July 2014.
- ^ Jump up to:a b c d e Knox, Dennis. “District Hospitals’ Important Mission”. Payers &–° Providers. Archived from the original on 14 July 2014. Retrieved 10 July 2014.
- ^ “Specialty Hospital Update” (PDF). National Public Radio. 2004. Archived from the original (PDF) on 18 July 2020. Retrieved 25 July 2020.
- ^ Jump up to:a b “Narayana Hrudayalaya Hospitals”. fastcompany.com. 7 February 2012. Archived from the original on 13 October 2013. Retrieved 13 October 2013.
- ^ “What’s a Teaching Hospital?”. www.brennerchildrens.org. Retrieved 13 June 2020.
- ^ “Hospital beds per 1,000 people”. Our World in Data. Retrieved 7 March 2020.
- ^ “The “virtual wards” supporting patients with covid-19 in the community”. BMJ. 2020 (369): m2119. 5 June 2020. Retrieved 24 December 2020.
- ^ “Modern technology reduces hospital admissions”. Building Better Healthcare. 2 December 2020. Retrieved 27 January 2021.
- ^ Legge, James (1965). A Record of Buddhistic Kingdoms: Being an Account by the Chinese Monk Fâ-Hien of his Travels in India and Ceylon (AD 399–414) in Search of the Buddhist Books of Discipline. Dev Publishers & Distributors.[page needed]
- ^ Arjuna Aluvihare, “Rohal Kramaya Lovata Dhayadha Kale Sri Lankikayo” Vidhusara Science Magazine, November 1993.
- ^ The American Journal of Islamic Social Sciences 22:2 Mehmet Mahfuz Söylemez, The Gundeshapur School: Its History, Structure, and Functions, p. 3.
- ^ Risse, G.B. Mending bodies, saving souls: a history of hospitals. 1990. p. 56
- ^ Ziegler, Tiffany A., Tiffany A. Ziegler, and Troyanos. Medieval Healthcare and the Rise of Charitable Institutions. Springer International Publishing, 2018, 33.
- ^ (Guenter Risse, Mending Bodies, Saving Souls: A History of Hospitals, 47–48).
- ^ Jan Pelikan, Jaroslav (13 August 2022). “Christianity: Curing and caring for the sick”. Encyclopædia Britannica.
- ^ Catholic Encyclopedia – [1] (2009) Accessed April 2011.
- ^ Byzantine medicine
- ^ Husain F. Nagamia, [Islamic Medicine History and Current practise], (2003), p. 24.
- ^ Glubb, Sir John Bagot (1969), A Short History of the Arab Peoples, retrieved 25 January 2008
- ^ Jump up to:a b “The Islamic Roots of the Modern Hospital”. aramcoworld.com. Retrieved 20 March 2017.
- ^ Islamic Culture and the Medical Arts: Hospitals, United States National Library of Medicine
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ^ Miller, Andrew C (2006). “Jundi-Shapur, bimaristans, and the rise of academic medical centres”. Journal of the Royal Society of Medicine. 99 (12): 615–617. doi:10.1177/014107680609901208. ISSN 0141-0768. PMC 1676324. PMID 17139063.
Another lasting advancement made during this time period was that of physician licensure. In 931 AD Caliph Al-Muqtadir learned that a patient had died in Baghdad as a result of a physician’s error. Consequently, he ordered Sinan ibn Thabit to examine all those who practiced the art of healing. Of the 860 medical practitioners he examined, 160 failed. From that time on, licensing examinations were required and administered in various places. Licensing boards were set up under a government official called Muhtasib, or inspector general. The chief physician gave oral and practical examinations, and if the young physician was successful, the Muhtasib administered the Hippocratic Oath and issued a license to practice medicine.
- ^ Alatas, Syed Farid (2006). “From Jami’ah to University: Multiculturalism and Christian–Muslim Dialogue”. Current Sociology. 54 (1): 112–32. doi:10.1177/0011392106058837. S2CID 144509355.
- ^ “Islamic Culture and the Medical Arts: Hospitals”. www.nlm.nih.gov. Archived from the original on 21 January 2024. Retrieved 21 January 2024.
- ^ Ikram, Sheikh Mohamad (1964). “Economic and Social Developments under the Mughals”. Muslim Civilization in India. Columbia University Press. p. 223. ISBN 978-0-231-02580-5.
- ^ Goldschmidt, Asaf (2023). “Reacting to Epidemics: The Innovative Imperial Public Health System during the Late Northern Song Dynasty”. Chinese Medicine and Culture. 6 (1): 68–75. doi:10.1097/MC9.0000000000000041.
- ^ The Royal Hospital Chelsea (Norwich: Jarrold Publishing, 2002), pp. 3–4
- ^ J. Bold, P. Guillery, D. Kendall, Greenwich: an architectural history of the Royal Hospital for Seamen and the Queen’s House (Yale University Press, 2001), pp. 4–7
- ^ “Colonial City of Santo Domingo. Outstanding Universal Value”. UNESCO World Heritage Centre website.
- ^ “Ruinas del Hospital San Nicolás de Barí”. Lonely Planet.
- ^ Williams, William Henry (1976). America’s First Hospital: The Pennsylvania Hospital, 1751–1841. Haverford House. ISBN 978-0-910702-02-7.
- ^ “NPGallery Digital Asset Management System: Pennsylvania Hospital”, National Register of Historic Places, National Park Service, retrieved 30 July 2019
- ^ “Painted window in St Bartholomew’s Hospital”. Archived from the original on 17 October 2021. Retrieved 7 June 2019.
- ^ Reinarz, Jonathan (2007). “Corpus Curricula: Medical Education and the Voluntary Hospital Movement”. Brain, Mind and Medicine: Essays in Eighteenth-Century Neuroscience. pp. 43–52. doi:10.1007/978-0-387-70967-3_4. ISBN 978-0-387-70966-6.
- ^ “General Acute Care Hospital in New York”. Archived from the original on 16 February 2023. Retrieved 6 October 2019.
- ^ Roderick E. McGrew, Encyclopedia of Medical History (Macmillan 1985), p. 139.
- ^ Freeman GK (2017). “Books: The Dispensaries: Healthcare for the Poor Before the NHS: Britain’s Forgotten Health-care System: Dispensaries: An Alternative to General Practice?”. Br J Gen Pract. 67 (655): 81. doi:10.3399/bjgp17X689281. PMC 5308110. PMID 28126876.
- ^ Michael Marks Davis; Andrew Robert Warner (1918). Dispensaries, Their Management and Development: A Book for Administrators, Public Health Workers, and All Interested in Better Medical Service for the People. MacMillan. pp. 2–3.
- ^ Surgeon Vice Admiral A Revell in http://www.histansoc.org.uk/uploads/9/5/5/2/9552670/volume_19.pdf Archived 6 November 2020 at the Wayback Machine
- ^ Waddington Ivan (1975). “The Development of Medical Ethics – A Sociological Analysis”. Medical History. 19 (1): 36–51. doi:10.1017/s002572730001992x. PMC 1081608. PMID 1095851.
- ^ Porter, Roy (1999) [1997]. The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present. New York: W.W. Norton & Company. pp. 316–17. ISBN 978-0-393-31980-4.
- ^ Kathy Neeb (2006). Fundamentals of Mental Health Nursing. Philadelphia: F.A. Davis Company. ISBN 978-0-8036-2034-6.
- ^ Nightingale, Florence (August 1999). Florence Nightingale: Measuring Hospital Care Outcomes. Joint Commission on Accreditation of Healthcare Organizations. ISBN 978-0-86688-559-1. Retrieved 13 March 2010.[permanent dead link]
- ^ Erna Lesky, The Vienna Medical School of the 19th Century (Johns Hopkins University Press, 1976)
- ^ Jump up to:a b c Emanuel, Ezekiel J. (25 February 2018). “Opinion | Are Hospitals Becoming Obsolete?”. The New York Times.
- ^ “Hospital Industry’s 10 Most Critical Metrics – Guiding Metrics”. guidingmetrics.com. Retrieved 25 November 2018.
- ^ “Fast Facts on U.S. Hospitals, 2018 | AHA”. 19 July 2024.
- ^ “As admissions have slumped and outpatient care booms, hospitals closing or shrinking”. Modern Healthcare. Retrieved 25 November 2018.
- ^ “Estimating Health Care-Associated Infections and Deaths in U.S. Hospitals, 2002” (PDF). Centers for Disease Control and Prevention. Archived from the original (PDF) on 15 October 2011. Retrieved 9 September 2023.
- ^ Jump up to:a b c “Two-Midnight and Observation Rule – Chicago Medical Society”. www.cmsdocs.org. Archived from the original on 25 November 2018. Retrieved 25 November 2018.
- ^ Jump up to:a b “CMS drops two-midnight rule’s inpatient payment cuts”. Modern Healthcare. Retrieved 25 November 2018.
- ^ “How U.S. Hospitals and Health Systems Can Reverse Their Sliding Financial Performance”. Harvard Business Review. 5 October 2017. Retrieved 25 November 2018.
- ^ Staff (11 April 2017). “5 common questions about micro-hospitals, answered”. www.beckershospitalreview.com. Retrieved 25 November 2018.
- ^ Jump up to:a b “When the tiny hospital can’t survive: Free-standing EDs with primary care seen as new rural model”. Modern Healthcare. 7 September 2011. Retrieved 14 May 2019.
- ^ Agnew, John (12 February 2010). “Deus Vult: The Geopolitics of Catholic Church”. Geopolitics. 15 (1): 39–61. doi:10.1080/14650040903420388. S2CID 144793259.
- ^ Calderisi, Robert. Earthly Mission – The Catholic Church and World Development; TJ International Ltd; 2013; p.40
- ^ “Catholic hospitals comprise one quarter of world’s healthcare, council reports :: Catholic News Agency (CNA)”. Catholic News Agency. 10 February 2010. Retrieved 17 August 2012.
- ^ Johnston, Martin (21 January 2008). “Surgery worries create insurance boom”. The New Zealand Herald. Retrieved 3 October 2011.
- ^ Jump up to:a b Hospitals in New Orleans see surge in uninsured patients but not public funds – USA Today, Wednesday 26 April 2006
- ^ Richmond, Barak D.; Kitzman, Nick; Milstein, Arnold; Schulman, Kevin A. (28 April 2017). “Battling the Chargemaster: A Simple Remedy to Balance Billing for Unavoidable Out-of-Network Care”. The American Journal of Managed Care. 23 (4). Retrieved 12 March 2023.
- ^ “Emergency Medical Treatment & Labor Act (EMTALA)”. Centers for Medicare & Medicaid Services. 26 March 2012. Retrieved 17 May 2013.
- ^ “CQC to inspect hospitals on food standards after patient deaths”. Health Service Journal. 17 November 2020. Retrieved 24 December 2020.
- ^ “Going into hospital far riskier than flying: WHO”. Reuters. 21 July 2011. Retrieved 27 January 2019.
- ^ Annmarie Adams, Medicine by Design: The Architect and the Modern Hospital, 1893–1943 (2009)
- ^ Jump up to:a b “Healing by design”. Ode. July–August 2006. Archived from the original on 17 October 2007. Retrieved 10 February 2008.
- ^ Yamaguchi, Yuhgo (5 October 2015). “Better Healing from Better Hospital Design”. Harvard Business Review. ISSN 0017-8012. Retrieved 30 August 2022.
- ^ Sample, Ian (20 February 2012). “Open hospital windows to stem spread of infections, says microbiologist”. The Guardian. Retrieved 12 March 2018.
- ^ Bowdler, Neil (26 April 2013). “Closed windows ‘increase infection'”. BBC News. Retrieved 12 March 2018.
- ^ “The psychological and social needs of patients”. British Medical Association. 7 January 2011. Archived from the original on 14 March 2011. Retrieved 14 March 2011.
- ^ Rosenberg, Julian (15 November 2004). “Health administrators go shopping for new hospital designs”. National Review of Medicine. Volume 1, no. 21. Archived from the original on 26 December 2008.